ST. LOUIS — Patricia Powers went a few years without health insurance and couldn’t afford regular doctor visits. So she had no idea cancerous tumors were silently growing in both of her breasts.
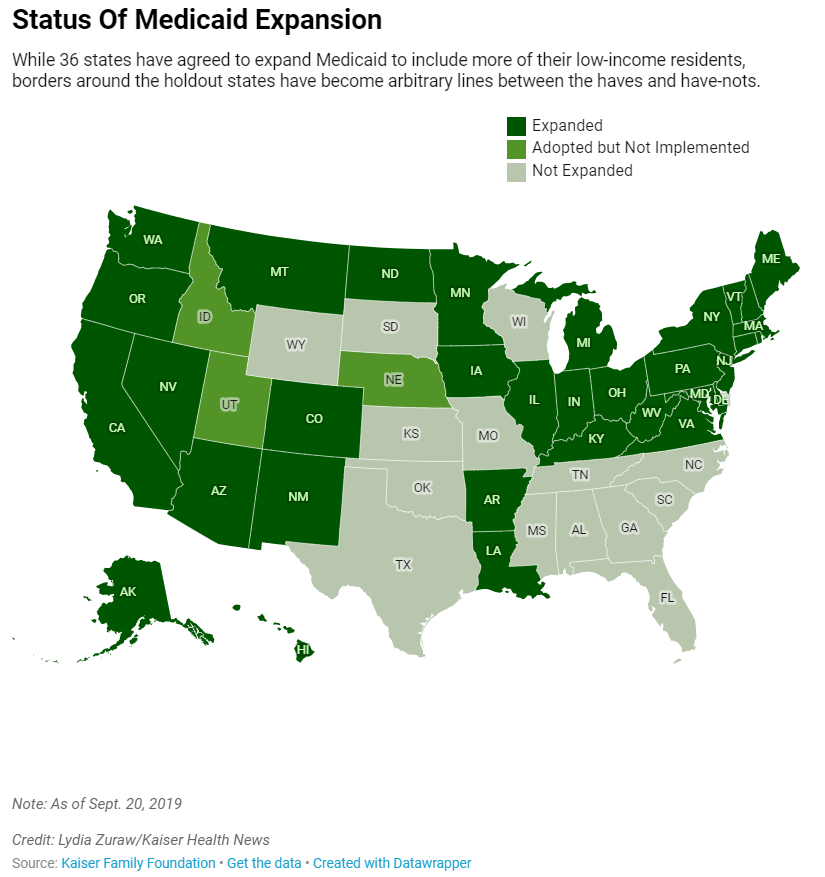
If Powers lived just across the Mississippi River in Illinois, she would have qualified for Medicaid, the federal-state health insurance program for low-income residents that 36 states and the District of Columbia decided to expand under the Affordable Care Act. But Missouri politicians chose not to expand it — a decision some groups are trying to reverse by getting signatures to put the option on the 2020 ballot.
Powers’ predicament reflects an odd twist in the way the health care law has played out: State borders have become arbitrary dividing lines between Medicaid’s haves and have-nots, with Americans in similar financial straits facing vastly different health care fortunes. This affects everything from whether diseases are caught early to whether people can stay well enough to work.
It wasn’t supposed to be this way. The ACA, passed in 2010, called for extending Medicaid to all Americans earning up to 138% of the federal poverty level, around $17,000 annually for an individual. But the U.S. Supreme Court in 2012 let states choose whether to expand Medicaid. Illinois did, bringing an additional 650,000-plus people onto its rolls. Missouri did not, and today about 200,000 of its residents are like Powers, stuck in this geographic gap.
Powers briefly thought about moving to another state, just to be able to get Medicaid. “You ask yourself: Where do you go? What do you do?” said Powers, who was in her early 60s when diagnosed. “Do I look at what’s happening in Illinois, right across the river?”
A recent University of Michigan study found Medicaid expansion substantially reduced mortality rates from 2014 to 2017. The researchers said Illinois averted 345 deaths annually while Missouri had 194 additional deaths each year. The same trends held for other side-by-side states such as Kentucky (did expand) and Tennessee (did not), New Mexico (did) and Texas (did not).
Dr. Karen Joynt Maddox, co-director of the Center for Health Economics and Policy at Washington University in St. Louis, said health care providers in her border city see how the coverage differences affect people. When treating Medicaid patients from Illinois, she said, doctors know procedures, equipment and medicines will likely be covered. With uninsured Missourians, they must consider whether patients can afford even follow-up medications after heart attacks.
Nonetheless, Medicaid expansion faces significant opposition in Missouri, a red state led by a Republican governor with GOP supermajorities in both legislative chambers.
Patrick Ishmael, director of government accountability for the Show-Me Institute, a Missouri free-market think tank, said offering Medicaid to people with incomes above the poverty level would drain resources from the state’s underserved poor and push up taxpayer costs. Though the federal government pays 90% of the cost of the expansion coverage, he said, Missourians contribute to that through their federal taxes. Medicaid already accounts for about a third of the state’s budget, which he said puts pressure on other priorities, like education.
“Missouri and other states need to think about whether they are a government that provides health care or a health care provider that sometimes governs,” he said.